CMS recently issued a final rule entitled “Patient Protection and Affordable Care Act; Updating Payment Parameters, Section 1332 Waiver Implementing Regulations, and Improving Health Insurance Markets for 2022 and Beyond.” The 341-page rule finalizes, without change, virtually all the provisions of the proposed rule, which was published on July 1, 2021.
Below we look at what these major provisions are and how they affect states operating on HealthCare.gov versus those running their own marketplaces.
- The annual Open Enrollment Period (OEP) for states operating on HealthCare.gov has been extended by one month, making the OEP November 1, 2021 to January 15, 2022. State-Based Marketplaces “with their own eligibility and enrollment platforms will be able to set their own annual Open Enrollment Period end dates, so long as these dates are on or after December 15, 2021.”
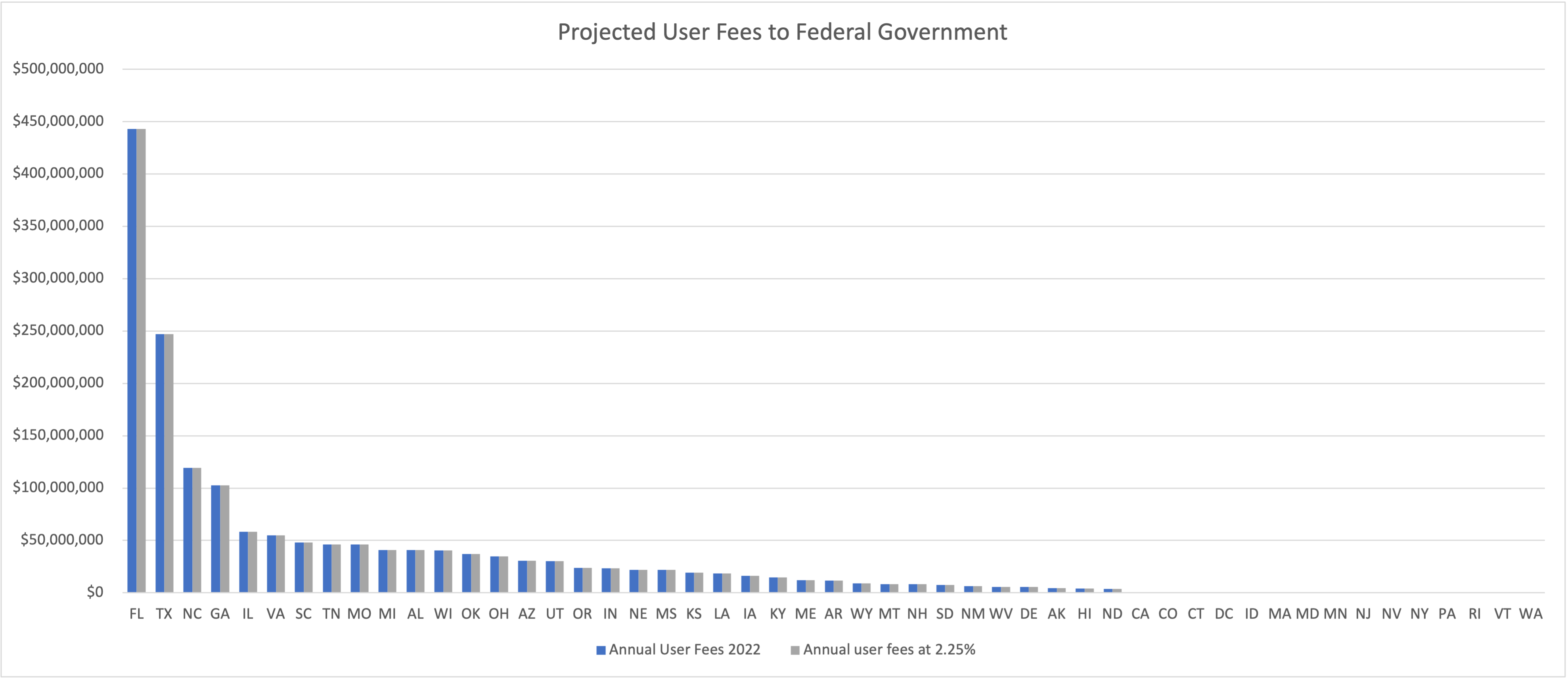
- The user fee has increased to 2.75 percent of premium per member, per month for states operating on HealthCare.gov, up from 2.25 percent. While this may not seem like a big change, for several states it means sending millions of additional dollars to the federal government, as compared to state-based marketplace (SBM) states, which are unaffected by the ruling and do not owe the federal government any portion of the PMPM premiums.
A comparison of 2.25 percent versus 2.75 based on August 2021 effectuated enrollments:
- The Exchange Direct Enrollment Option for states has been repealed. This had allowed states to work directly with private sector entities such as web-brokers to serve as the consumer-facing front-end of the exchange, in place of a government-run website. (As was requested in a waiver by the state of Georgia.) Several concerns had been raised about this model, including the transparency of plan available if working without a platform (such as state based marketplace) in place.
- HealthCare.gov will establish a monthly special enrollment period (SEP) for qualified individuals with household incomes at or below 150 percent of the Federal Poverty Level (FPL). This is an optional measure for SBM states. It is worth noting, however, that this rule is only applicable while American Rescue Plan (ARP) expanded subsidies are in place. If they do not get extended, this SEP provision will go away.
- The separate billing requirement that issuers needed to send a separate bill for abortion services in accordance with section 1303 of the ACA has been repealed. For SBMs this could alleviate any compliance monitoring, but this is an issuer requirement to do separate billing for non-Hyde abortion services, more so than anything directly impacting HealthCare.gov or SBM operations.
- State flexibility limitations established under the Trump Administration for section 1332 State Innovation Waivers have been repealed. The repeal of the 2018 regulations will give states more flexibility when applying for a 1332 waiver. States can explore innovative ways to provide better access to care, lower the cost of coverage, and decrease costs to the federal government.
Want to learn more about ways a state-based marketplace can benefit your state and its health insurance market? We’re here to help.