Back in the day, 2005 that is, our goal was to service consumers directly, to be the “Expedia of health insurance.” In other words, our founders wanted to make it simple for people to understand what they were signing up for when they were shopping for a health insurance plan so they could make better, more informed decisions. If you don’t know what “premium”, “copay”, “deductible”, and “cost sharing” mean, the odds of you selecting an appropriate plan are pretty low. We wanted to help. And we did; that first year we helped roughly 5,000 people enroll.
After the passage of the Affordable Care Act (ACA), we began to realize that to continue growing – and more importantly, to continue helping as many consumers as possible – we had to change our business model and shift our focus to working with the states that were building health insurance exchanges. And from there, it’s history, as they say.
Today, GetInsured’s technology is currently being leveraged, in five states – California, Idaho, Minnesota, Nevada, and Washington. Our solutions give states new opportunities to improve their consumer experience versus their bespoke legacy systems that tend to be expensive to maintain and difficult to scale. We’ve proven that having a cloud-based system power health exchanges dramatically reduces its cost, increases flexibility, allows us to conform to each state’s individual needs, and is a prime reason why GetInsured is a leading state exchange platform provider today.
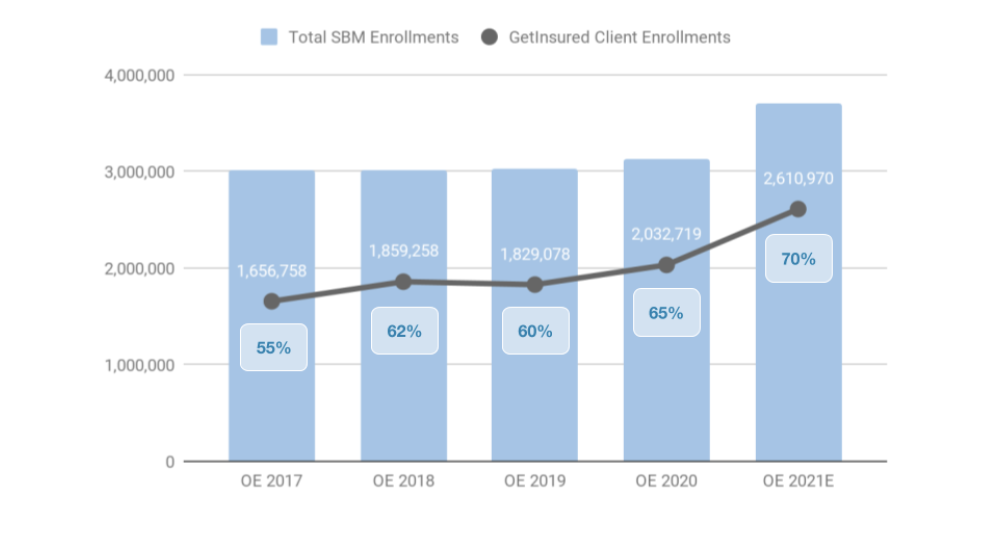
Once we onboard Pennsylvania and New Jersey for this year’s open enrollment period, GetInsured’s technology will reach 70 percent of all state-based marketplaces, with more than 2.6 million enrollments, making the company the clear market leader. We couldn’t be happier that an idea back in 2005 turned into a platform that is making plan selection easier for millions of people across the country.