CMS announced on September 10, 2021, that it would be “awarding $20 million in American Rescue Plan (ARP) grant funding to State-based Marketplaces (SBMs) to increase consumer access to affordable, comprehensive health insurance coverage.” States that applied for these grants have been awarded funds that allow for the modernization of IT systems and/or to conduct targeted consumer outreach activities.
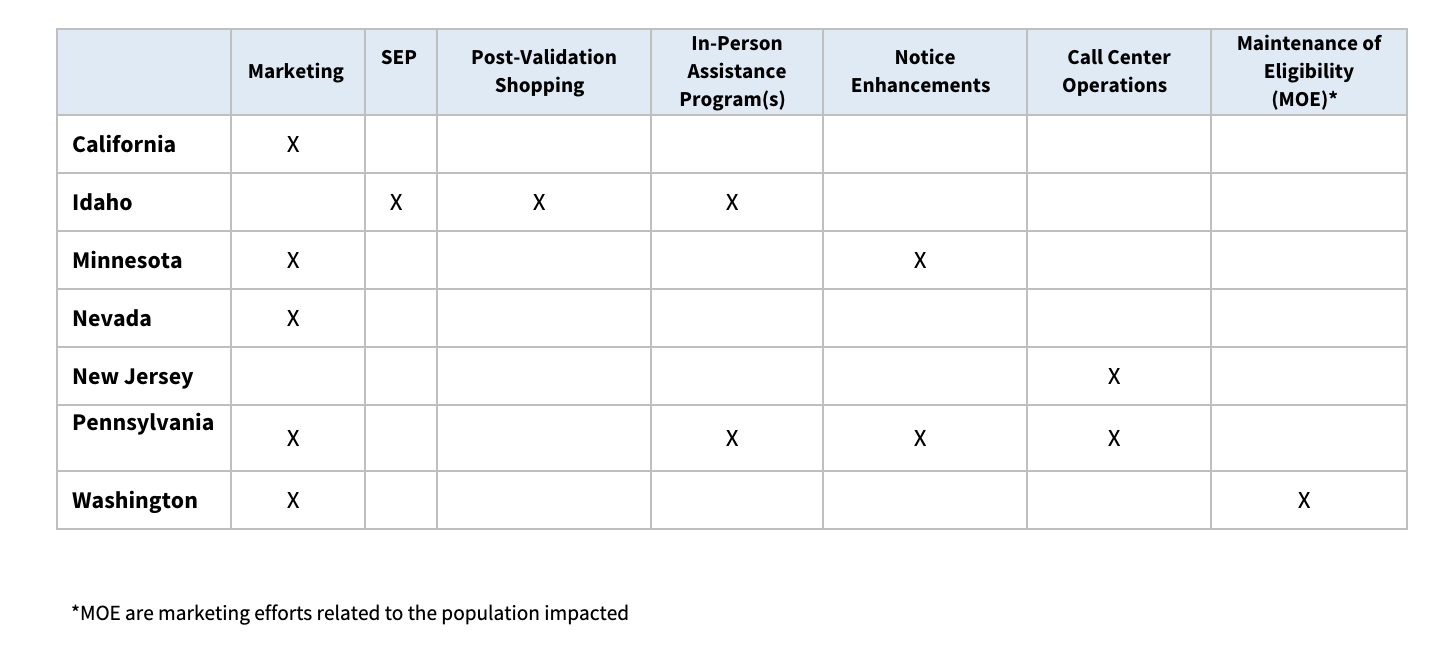
Nearly 40% ($7.7 million) of the $20 million were awarded to the seven GetInsured’s state clients. Here’s a look at what each state plans to do with their grant money.
California: California Health Benefit Exchange (Covered California): $1,107,392.87
Covered California proposes to develop and produce a robust ARP consumer education campaign featuring the tagline “This way to health insurance” that centers on the experiences of real Californians who’ve struggled to get health insurance in the past.
- The campaign will build brand awareness and engagement, educate consumers about the availability of new ARP subsidies, drive enrollment, and reflect the state’s ethnically diverse population.
- The campaign will reach California’s ethnically diverse population via cost-effective means to ensure Californians are aware of new subsidies available to them via the ARP, while also building brand awareness and engagement and driving enrollment through Covered California.
- The campaign will be targeted to reach consumers across various cultures and languages between the ages of 25-64 with a minimum household income of $25,000 and will be specifically used to reach consumers in the multicultural segment.
Idaho (Your Health Idaho): $1,107,392.87
- Your Health Idaho (YHI) proposes to use funding to modernize Marketplace technology, including making key updates to improve the customer experience for Idahoans seeking to enroll through a Special Enrollment Period (SEP), allowing consumers to shop for plans while their Qualifying Life Event (QLE) documents are reviewed and validated, and modernizing technology controls to allow more flexibility to remove or merge multiple household applications.
- YHI proposes to use funding to modernize and enhance support for in-person assisters and enrollment counselors who are critical to educating Idahoans about their enrollment options and the benefits of ARP, as well as serving Idaho’s most vulnerable populations.
- YHI also proposes to use a portion of the funding for costs related to updating necessary systems and technology to provide increased financial assistance through the ARP.
Minnesota (MNsure): $1,107,392.87
- MNsure proposes to modernize and update Marketplace systems and technology, and to implement and operate the amendments to the APTC and cost-sharing reduction (CSR) programs made by sections 2305, 9661, and 9663 of the ARP.
- MNsure plans to update and improve the annual notice used to inform consumers about household eligibility for enrolling in coverage for the coming plan year and develop a new notice to inform and assist consumers who are approaching age 65 and planning to enroll in Medicare to help avoid dual enrollment and dual billing situations.
- Additionally, MNsure proposes a statewide consumer education and outreach campaign to increase awareness of ARP benefits and drive enrollment.
Nevada (Silver State Health Insurance Exchange/Nevada Health Link): $1,046,499.81
- The Silver State Health Insurance Exchange (SSHIX) proposes to use funding for the costs associated with helping Nevada consumers realize the savings available to them under the ARP, which includes implementing eligibility and enrollment system changes and increasing call center capacity to ensure consumers can get help when they needed it.
- SSHIX also proposes to develop and implement a comprehensive consumer education and outreach campaign to ensure consumers are aware of the new benefits available under the ARPA.
- SSHIX proposes to target uninsured and underinsured Nevadans, as well as existing Nevada Health Link consumers.
New Jersey (Get Covered New Jersey): $1,107,392.87
- The New Jersey Department of Banking and Insurance (DOBI) proposes to use funding help cover the costs of the technical implementation of the ARP benefits, including changing APTC amounts and automatically updating already enrolled consumers with the expanded financial help.
- DOBI proposes to expand its call center operations and capacity in response to an anticipated significant increase in call volume due to the increased financial help made available through ARP. The focus will be on existing enrollees who can benefit from increased financial help and new consumers that may be newly eligible for financial help. DOBI’s call center expansion will mean more customer service representatives that are well-trained to be able to answer consumer questions quickly and 2021 State Marketplace Modernization Grant Awards 9/10/2021 accurately without long wait times.
- DOBI also plans to expand call center support for processing and resolving data matching issues and will make updates to call center processes, scripts, and system to ensure that customer service representatives are trained on the nuances of ARP.
Pennsylvania (Pennsylvania Health Insurance Exchange Authority/Pennie): $1,107,392.87
- The Pennsylvania Health Insurance Exchange Authority (d/b/a Pennie) proposes to use funding to support two consumer-centric projects that facilitate exposure of the ARP benefits, including expanded call center support and increased consumer assistance. Pennie’s consumer assistance center significantly increased its staffing and support this year, based on anticipated pressure stemming from the ARP campaign, a comprehensive outreach campaign, distribution of approximately 240,000 eligibility notices, and email prompts.
- Pennie also proposes an enhancement to, and expansion of, its Exchange Assister program to specifically target historically under and uninsured populations. Pennie proposes to add subcontractors already aligned with Pennie’s goals and serving the LGBTQ, Hispanic/Latino, and African American communities. Exchange Assisters will work with consumers through community centers and one-on-one appointments, as well as an amplified calendar of outreach and educational events.
Washington (Washington Health Benefit Exchange/WAHBE): $1,107,392.87
In order to update its systems and successfully implement provisions of the ARP, the WAHBE is proposing a two-pronged project.
- The first initiative is aimed at addressing consumer education challenges, particularly in Washington’s underserved rural and urban communities. WAHBE will conduct statewide educational and outreach events to reach these communities and specifically target the uninsured, those currently enrolled in Medicaid who may lose eligibility at the end of the COVID-19 Public Health Emergency, and current customers who are receiving expanded COBRA premium subsidies which are set to expire.
- The second initiative will address the technical challenges of implementing ARP provisions on Washington Healthplanfinder. WAHBE proposes to enhance the Washington Healthplanfinder and respond to system limitations further exacerbated by ARP with the goal of increasing system enhancement capacity, enabling the WAHBE to meet ongoing business needs, as well as address new needs necessary for the successful implementation and operation of ARP in Washington.