Nevada Health Link enrolled 6,017 Nevadans during its limited-time Exceptional Circumstance Special Enrollment Period (ECSEP) in response to COVID-19. The ECSEP — which ran from March 17 to May 15, 2020 — was opened to allow qualified Nevadans who missed OEP to secure health care coverage.
Standard SEPs—which allow for change of income, loss of a job, or moving—are already in the GetInsured system and our customer service reps are routinely trained to handle them. In the case of Nevada’s ECSEP, COVID as a reason wasn’t baked into the system or training, so reps had to be brought up to speed on additional qualifying life events (QLE) for opening an SEP. Our Nevada Health Link consumer assistance center operations were apprised of the ECSEP on March 15 and our CSRs were trained by March 17. In a perfect storm kind of situation, due to the pandemic, the consumer assistance center operations also transitioned to a remote force shortly after the ECSEP went live.
Apart from being trained on the deadlines, effective dates, and eligibility requirements, the team received extensive sensitivity training. In circumstances like COVID, consumers tend to believe that anything impacting them is a life event. However, where health insurance is concerned, every life event doesn’t necessarily translate into a qualifying life event with eligibility to enroll. So, our CSRs were trained to uncover as sensitively as possible if a consumer’s situation truly qualified for the ECSEP, with the goal of trying to get the maximum number enrolled.
The ECSEP was comparable to the first two weeks of regular season open enrollment. The table below compares the call volumes, service levels average handle times, and abandon rates between Nevada Health Link’s OEP for the 2020 Plan Year and the ECSEP.
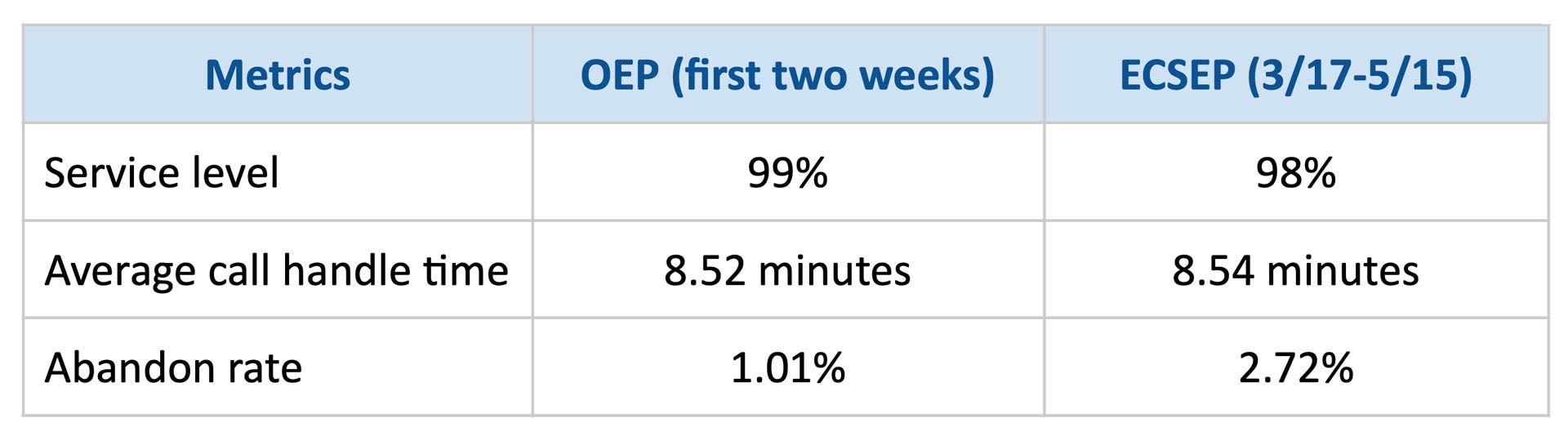
The result speaks for itself — our customer satisfaction score for the ECSEP was 91.77%.